If you’ve been referred for a nerve conduction study, you may be feeling two things at once: curiosity and concern. Symptoms like numbness, tingling sensations, or muscle weakness can be unsettling, especially when they affect your work, sleep, or daily comfort. Many patients also worry about whether the test will be painful, how long it takes, and what the test results might mean for their diagnosis.
A nerve conduction study is one of the most common diagnostic tests used to evaluate how well your peripheral nervous system is sending electrical signals along a nerve pathway. Because nerves control sensation and movement, changes in signal speed or strength can help your clinician understand whether symptoms are more consistent with peripheral neuropathy, peripheral nerve damage, or another category of nerve disorders.
At BluePoint Medical Group, we approach these evaluations with a patient-first mindset. The goal is not only to run tests, but to connect your symptoms, your medical history, and any related findings into a clear, actionable plan—without exaggeration, guarantees, or one-size-fits-all conclusions.
When Numbness, Tingling, or Weakness Raises Concern About Nerve Disorders
Many people start noticing symptoms gradually—mild hand tingling, intermittent foot numbness, or a subtle loss of grip strength. Even when symptoms feel minor, they can reflect changes in how peripheral nerves are functioning, especially if the pattern persists or spreads to the legs or both sides of the body.
A conduction study can be useful because it focuses on measurable function rather than guesswork. By assessing how a nerve signal travels, the test can help clarify whether your symptoms are more consistent with a localized issue (like carpal tunnel syndrome involving the median nerve) or a broader condition affecting multiple nerves.

Is a Nerve Conduction Test a Good Fit for Tingling or Muscle Weakness?
A nerve conduction test is often ordered when symptoms suggest the nerves may not be transmitting signals normally. This can include persistent tingling, weakness, burning sensations, or reduced sensation in the hands or feet. It can also be considered when a clinician suspects muscle and nerve disorders that affect function over time.
The test is especially helpful when the exam suggests involvement of motor nerves (which support movement) or sensory nerves (which support feeling). Because many different conditions can cause similar symptoms, objective testing can support a more confident approach to diagnosis and next steps.
Do I Need Blood Tests or Urine Tests Before a Nerve Conduction Study?
Some patients need only the nerve study, while others may have blood tests or urine tests as part of a broader evaluation. Those labs don’t replace the nerve test; they can help identify contributors to symptoms such as metabolic changes, inflammation, vitamin deficiencies, or other factors that may affect nerve function.
Your healthcare provider may recommend labs based on your symptoms, risk factors, and medical background. This is one reason it helps to share your full medical history, including medications, recent illnesses, and how long symptoms have been present.
What a Nerve Conduction Study Measures: Electrical Activity and Nerve Signal Pathways
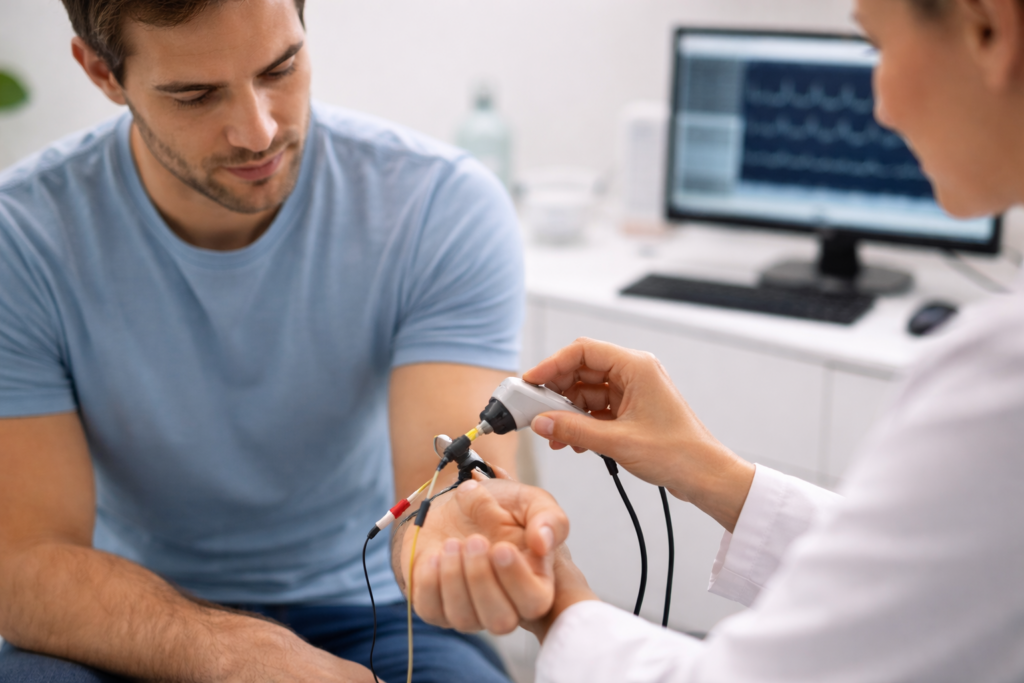
A nerve conduction study measures how quickly and how strongly a nerve carries electrical impulses. During the test, the clinician uses electrical stimulation to briefly stimulate a nerve and then records the response downstream. This helps evaluate how signals move through the peripheral nervous system.
It’s important to know what the test does and does not do. It does not directly image the brain or the brain and spinal cord, and it doesn’t diagnose every neurological condition by itself. Instead, it focuses on how electrical activity travels through peripheral nerves, which can be highly relevant for suspected nerve compression or peripheral nerve injury.
How Electrical Stimulation Creates Small Electrical Impulses During Testing
During the test, electrode patches or small electrodes are placed on the skin over specific nerve locations. The clinician may stick electrodes (adhesive sensors) to the skin and use a separate stimulator to deliver electrical pulses—each one a small electrical impulse designed to be brief and controlled.
The sensation is often described as a quick tapping or a mild tingling feeling. Some patients describe a short “zap,” while others mainly notice a tingling sensation that fades quickly. The goal is to produce consistent electrical signals so the equipment can measure the nerve’s response accurately.
What Is Nerve Conduction Velocity and Why Does Speed Matter?
Nerve conduction velocity refers to how fast the signal travels along the nerve. If the signal is slower than expected, it may suggest a problem with the nerve’s insulation (myelin) or a conduction block. If the signal is weaker than expected, it may suggest nerve damage affecting the nerve fibers themselves.
This “speed and strength” view can help your clinician interpret patterns across nerves. For example, if one nerve shows changes but the next nerve tested looks normal, that pattern can point toward a focal compression rather than widespread neuropathy. Patients often ask, “How many nerves will you test?”—and the answer varies based on symptoms and exam findings.
How Peripheral Nerves Connect to the Spinal Cord and the Nervous System
Your spinal cord acts like a central highway for signals traveling between the body and the brain, but many symptoms start “downstream” in the peripheral nervous system. When peripheral nerves aren’t carrying messages properly, you may notice changes in sensation, reflexes, strength, or coordination—even when the brain itself is not the primary problem.
Understanding this distinction matters because it shapes which tests are most useful. A nerve conduction evaluation helps map the functional integrity of the nerve pathway outside the central nervous system. If a clinician is concerned about a central issue involving the brain and spinal cord, they may recommend other tests based on the full clinical picture.
Which Nerve Disorders Can a Conduction Study Help Evaluate?
A conduction study may help evaluate patterns consistent with peripheral neuropathy, localized nerve entrapment, or peripheral nerve damage related to injury or compression. It may also support evaluation for certain inherited or progressive conditions, such as charcot marie tooth disease, where peripheral nerve function can change over time.
In other scenarios, the test can assist with evaluating symptoms that overlap with broader neurological disorders. For example, clinicians may consider it when symptoms raise questions about guillain barré syndrome or motor neuron disease (often discussed by patients as Lou Gehrig’s disease). Importantly, the study is interpreted alongside your exam and history—never as a standalone “final answer.”
How Is It Different From an EMG Test or Electromyography EMG?
Patients often hear about the emg test alongside nerve conduction testing. Electromyography (EMG) evaluates muscle electrical signals and can help assess whether symptoms are more related to a nerve issue, a muscle disorder, or the connection between nerve and muscle. In many cases, clinicians order both tests because they answer different questions.
Unlike the conduction portion, EMG typically uses a small needle to record muscle activity, which may feel different than surface electrodes. While it can cause brief discomfort, many patients tolerate it well, and it can add valuable context when there are weakness, atrophy concerns, or complex symptom patterns.
What to Expect During a Nerve Conduction Study in an Outpatient Setting
Most nerve conduction studies are done in an outpatient setting, meaning you come in, complete the test, and go home the same day. You’ll usually be asked to sit or lie comfortably while the clinician places electrodes and runs a sequence of stimulations. Clothing access matters, so sleeves or pant legs that can be adjusted may be helpful depending on symptom location.
The clinician may test a set of nerves relevant to your symptoms—sometimes starting with the most symptomatic area and then comparing responses on the other side. If your symptoms involve your hands, the median nerve and other nearby nerves may be tested. If symptoms involve feet or legs, the test may focus on lower extremity nerves and related pathways.
How the Electrodes Work: One Electrode, Then the Next Nerve
You’ll typically see electrodes placed in a pattern: one electrode records the response, while stimulation occurs at a measured distance away. In simple terms, the test uses timing and distance to evaluate signal speed. This is why the placement and measurement process can feel methodical and precise.
As the clinician moves from one nerve to the next, they are looking for patterns—how the same type of stimulation produces different responses across nerves. That comparison can be clinically meaningful, especially when differentiating focal entrapment from generalized neuropathy.
Does It Hurt, and What Does Minor Discomfort Feel Like?
Most patients report minor discomfort rather than severe pain. The stimulation can cause a brief jolt or twitch, and some people experience minor discomfort from the intensity needed to capture a clear signal. A transient mild tingling feeling is common and typically resolves immediately after each pulse.
If you have severe pain, high anxiety about procedures, or a history of sensitivity to electrical stimulation, tell your healthcare provider beforehand. Your team can explain what to expect, adjust pacing, and help you stay as comfortable as possible while still collecting useful data.

How Test Results Support Diagnosis and a Treatment Plan for Many Different Conditions
Your test results can help clarify whether symptoms are more consistent with nerve compression, demyelination, axonal injury, or other functional changes. This information can support the clinical diagnosis, especially when symptoms overlap across conditions. It can also help guide a plan that may include activity adjustments, splinting, therapy, medication review, or referrals, depending on findings.
The most important value of a nerve conduction evaluation is direction. When clinicians understand where the signal is disrupted, they can focus care more precisely. For example, if findings support carpal tunnel syndrome, your plan may focus on wrist positioning and nerve protection. If findings support broader neuropathy, the plan may include further evaluation for metabolic or systemic causes.
When Other Tests Like CT Scan, Blood, or Urine Tests May Be Considered
Sometimes, clinicians recommend other tests to complete the picture. For example, a ct scan may be relevant if there’s concern about structural issues affecting a region, though CT is not a direct nerve function test. More commonly, additional blood work or urine tests may be used to evaluate contributing factors that can affect nerves.
The key is alignment: each test should answer a specific question. If a test won’t change the plan, it may not be necessary. A good preventive and diagnostic approach focuses on clarity, appropriate use of resources, and avoiding excessive testing.
FAQ
Is a nerve conduction studynon-invasivee?
A nerve conduction study is generally considered non-invasive because it uses surface electrodes on the skin rather than surgical procedures. You may feel brief electrical pulses, but the test typically does not break the skin during the conduction portion.
How long does a nerve conduction test take, and will it test many nerves?
Timing depends on symptoms and how many nerves are evaluated, but many studies take under an hour. Your clinician chooses how many nerves to test based on your exam and whether comparison testing is needed across the arms, hands, or legs.
Should I be worried if I have pain or tingling during electrical stimulation?
A brief tingling or twitch is expected during electrical stimulation, and most patients report only mild discomfort. If you have severe pain, worsening symptoms afterward, or concerns about sensitivity, let your provider know so the plan can be adjusted and interpreted appropriately.

Conclusion
If your symptoms include persistent numbness, tingling, weakness, or functional changes, a thoughtful evaluation can help you move from uncertainty to a plan. A nerve conduction study can be a helpful step, especially when paired with a careful history and exam that considers your daily activities, health conditions, and risk factors.
If you’re scheduled for a nerve conduction study or wondering whether it’s appropriate, contact BluePoint for next steps and schedule a consultation. We’ll review your symptoms, discuss what the test can show, and help you understand how results may inform a safe, individualized treatment plan.
Results vary, and testing decisions should be personalized based on your medical history and clinical findings.
