Many patients visiting a primary care provider wonder whether an EKG test is something they should expect during a routine appointment. Questions often arise when symptoms like chest pain, shortness of breath, or heart palpitations appear—or when there is concern about underlying heart disease due to age or family history. Because heart conditions can develop silently, it’s natural for patients to want reassurance through diagnostic testing.
At BluePoint Medical Group, primary care focuses on prevention, early detection, and informed decision-making. An electrocardiogram (EKG or ECG) is one of several tools doctors may use to assess heart health, but it is not automatically performed at every visit. Understanding when an EKG is considered routine—and when it is not—helps patients feel more confident discussing testing with their doctor.
This article explains whether an EKG is a routine test in primary care, what it evaluates, and how it fits into personalized, preventive medical care.
Understanding What an EKG Measures in Primary Care
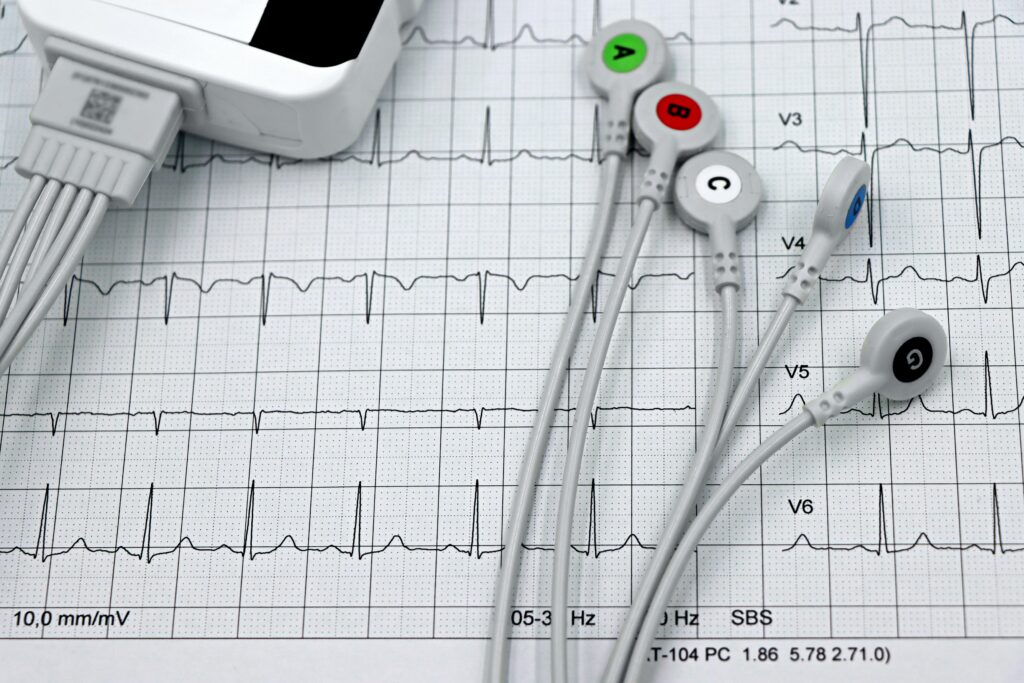
An EKG is a non-invasive, painless test that records the heart’s electrical activity. Using small sticky patches placed on the skin, the test captures electrical signals that show how the heart beats and whether its rhythm is regular.
For patients, this matters because the heart relies on precise electrical impulses to pump blood effectively through the cardiovascular system. Disruptions in these signals may indicate irregular heartbeats, prior heart damage, or other heart conditions.
In primary care, an EKG serves as a snapshot of the heart’s activity at a specific moment. It does not diagnose every heart problem, but it can reveal patterns that guide further evaluation.

Are EKGs Considered Routine in Primary Care Visits?
In most cases, routine EKGs are not automatically performed on all patients during annual checkups. For most people, especially younger adults without symptoms or known risk factors, a physical exam and medical history provide sufficient initial assessment.
However, doctors may get an EKG as part of routine care for older adults or patients at higher risk for heart problems. This includes individuals with high blood pressure, high cholesterol, diabetes, or a strong family history of cardiovascular disease.
Understanding this distinction helps patients avoid unnecessary testing while still ensuring appropriate monitoring based on personal risk.
Symptoms That May Prompt a Primary Care EKG
A primary care doctor may recommend an EKG when patients report heart-related symptoms such as chest pain, shortness of breath, dizziness, or a racing or irregular heartbeat. Symptoms like chest pain and shortness of breath may raise concern for potential heart issues that warrant immediate assessment.
An EKG can help determine whether symptoms are likely related to the heart’s rhythm or electrical activity, or whether other causes should be explored. This initial insight can prevent delays in care and support timely next steps.
For patients, symptom-driven testing ensures that diagnostic decisions are responsive and clinically appropriate.
Risk Factors That Influence the Need for an EKG
Doctors often consider an EKG for patients with specific risk factors, even if they feel well. These include age, smoking history, diabetes, obesity, or previously diagnosed heart disease.
Patients with a previous heart attack or known heart problems may have regular EKGs to monitor changes over time. Comparing current EKG results with past recordings helps assess progression or stability. This risk-based approach allows primary care providers to balance prevention with practicality.
How an EKG Fits Into Preventive Heart Health Care
In preventive medicine, an EKG is one tool among many used to assess cardiovascular risk. Blood tests, blood pressure readings, lifestyle review, and symptom discussion are equally important in evaluating heart health.
For patients, this means an EKG is rarely used in isolation. Instead, it complements other data to provide a fuller picture of cardiovascular status. This integrated approach supports thoughtful prevention rather than reliance on a single test.

What the EKG Process Is Like for Patients
An EKG is usually completed in a short amount of time during a routine office visit. Small adhesive sensors are gently applied to specific areas of the body, allowing the test to capture how the heart’s electrical activity moves through the chest and limbs.
The test is non-invasive, does not involve needles, and does not deliver electricity into the body. Patients can breathe normally and do not need special preparation.
Knowing what to expect helps reduce anxiety and encourages patients to feel comfortable when testing is recommended.
Interpreting EKG Results in Primary Care
After the test, the doctor will review the EKG to evaluate heart rate, rhythm, and waveform patterns. Results may appear normal, abnormal, or inconclusive.
Abnormal findings do not always indicate serious disease. Sometimes variations reflect benign differences or temporary changes. However, certain patterns may suggest hidden problems that require further testing. For patients, understanding that EKG findings are interpreted in context prevents unnecessary alarm.
When an EKG Leads to Additional Testing
If EKG results raise concern, a primary care provider may recommend additional evaluation, such as a stress test, heart imaging, or referral to cardiology. This stepwise process ensures accuracy before treatment decisions are made.
Patients experiencing ongoing symptoms or worsening signs may need closer monitoring or specialized testing to determine the cause. This careful progression avoids overtreatment while ensuring safety.
Limitations of EKGs Patients Should Understand
While useful, an EKG does not detect every heart condition. Some problems occur intermittently or only during exercise, which may not appear on a resting test.
Normal EKG results do not completely rule out heart disease, especially in early stages. This is why symptoms and risk factors remain central to decision-making. Realistic expectations help patients appreciate both the value and limits of EKG testing.
How Primary Care Providers Decide if You Need an EKG
Primary care doctors consider symptoms, medical history, exam findings, and overall risk when deciding whether a patient needs an EKG. This individualized approach aligns testing with clinical relevance.
Patients are encouraged to share concerns openly, especially changes in exercise tolerance, new chest discomfort, or unexplained fatigue. Shared decision-making ensures testing is appropriate and patient-centered.
Benefits and Considerations for Patients
An EKG can provide reassurance, establish a baseline, or identify issues that require attention. When used appropriately, it supports early detection and informed care planning.
However, unnecessary testing may lead to anxiety or additional procedures without a clear benefit. Understanding why a test is recommended is key. Patients benefit most when EKGs are usedthoughtfully within comprehensive primary care.
FAQ
Is an EKG always part of a routine checkup?
No. EKGs are not routinely performed for all patients and are usually recommended based on symptoms or risk factors.
When should I ask my doctor about getting an EKG?
You should ask if you experience chest pain, shortness of breath, palpitations, or have concerns due to family history or chronic conditions.
How long does an EKG take?
The test typically takes only a few minutes and is performed in the office.
Can a normal EKG rule out heart disease?
Not completely. A normal EKG does not exclude all heart conditions, which is why overall evaluation is important.
Conclusion
Understanding whether an EKG is a routine test in primary care helps patients approach cardiovascular screening with clarity rather than confusion. While EKGs are not automatically performed at every visit, they play an important role for patients with symptoms, risk factors, or known heart conditions. When used appropriately, an EKG offers valuable insight into the heart’s rhythm, electrical activity, and overall cardiovascular status.
It’s important to remember that individual needs vary, and no single test defines heart health on its own. EKG results must be interpreted alongside medical history, physical exams, and other diagnostic information. This balanced approach supports accurate diagnosis and avoids unnecessary testing.
At BluePoint Medical Group, primary care emphasizes personalized evaluation and preventive decision-making. Scheduling an appointment allows patients to discuss symptoms, risk factors, and whether an EKG or other testing is appropriate for their individual health needs.
